Mental health issues, changing hormones and a higher risk for sleep disorders can all impact how long and how well you sleep.
Most adults need seven to nine hours of sleep per night. And while everyone’s sleep needs are different, women tend to get the short end of the stick when it comes to the duration and quality of sleep.
Studies show that women have more trouble falling and staying asleep than men1, but our bodies actually need more sleep than theirs do.2 Let’s have a look at some of the factors that affect our sleep, and what you can do to change them.
- We’re wired differently.
Women are 40% more likely than men to experience insomnia.3 Whether it’s work worries or family and caregiver responsibilities, our minds often begin to race the minute our heads hit the pillow. - Our hormones don’t help.
Hormonal shifts during the menstrual cycle, especially in the days leading up to menstruation, can disrupt sleep. (There’s actually a name for it: period insomnia.) As our estrogen and progesterone levels fluctuate during perimenopause, these fluctuations can impact the quality and duration of our sleep. - We experience more sleep disorders.
The risk for some sleep disorders, including restless legs syndrome, is twice as high for women as men. Up to 67% of postmenopausal women have obstructive sleep apnea, causing snoring that can further disrupt sleep.4 - We often put off bedtime for me time.
When you’re caring for kids or an elderly loved one, your alone time is precious. To ensure we actually get some, we often put off going to sleep to fit some me time into our days. Some call it “revenge bedtime procrastination (RBP),” the culprit of many a sleep issue.
Women are more likely to experience stress, anxiety and depression, which can contribute to sleep problems. The opposite is also true: if you’re not sleeping, it can make your anxiety or depression feel overwhelming.
Here’s a closer look at some common concerns women face.
Anxiety and stress
Both anxiety and stress can trigger the release of hormones such as cortisol, which can make it difficult to relax and fall asleep. Even when we do fall asleep, the racing thoughts we often have swirling in our heads can wake us up in the middle of the night, with little hope of falling back asleep.
Depression
It may come as no surprise that depression and sleep problems are also closely linked. Here are some staggering facts:
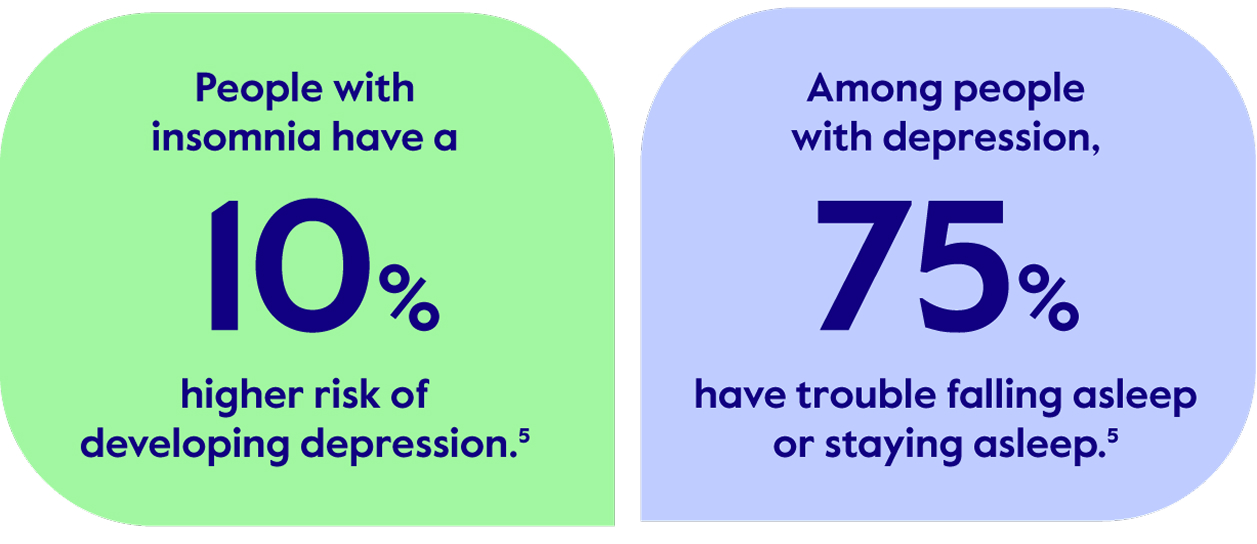
Symptoms of depression in women can vary in intensity and duration. Common symptoms include feelings of hopelessness, helplessness, loss of interest or pleasure in hobbies and activities, changes in sleep or appetite, and more.
Neurodivergence
Conditions such as attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD) and even dyslexia can make it difficult to turn your brain off at night and get the sleep you need. This lack of sleep can worsen daily activities, such as planning, organization and impulse control. If you’re on certain medications, such as stimulants, those can also disrupt sleep.
Having trouble falling and staying asleep can impact your overall well-being. Not to mention the toll it can take on your physical health. Keep reading for tips and resources that can help.
Sleep tip
Receiving support for a mental health concern can be the first step to improving your sleep. Try 24/7 virtual therapy to connect by phone or video without leaving home.
As if going through perimenopause weren’t challenging enough, the hormonal changes you experience in your 40s and 50s can cause sleepless nights—and daytime fatigue. Perimenopause can impact your circadian rhythm, mood and more, all of which can disrupt your sleep.
If you’re experiencing sleep disorders at this stage in your life, you’re not alone.
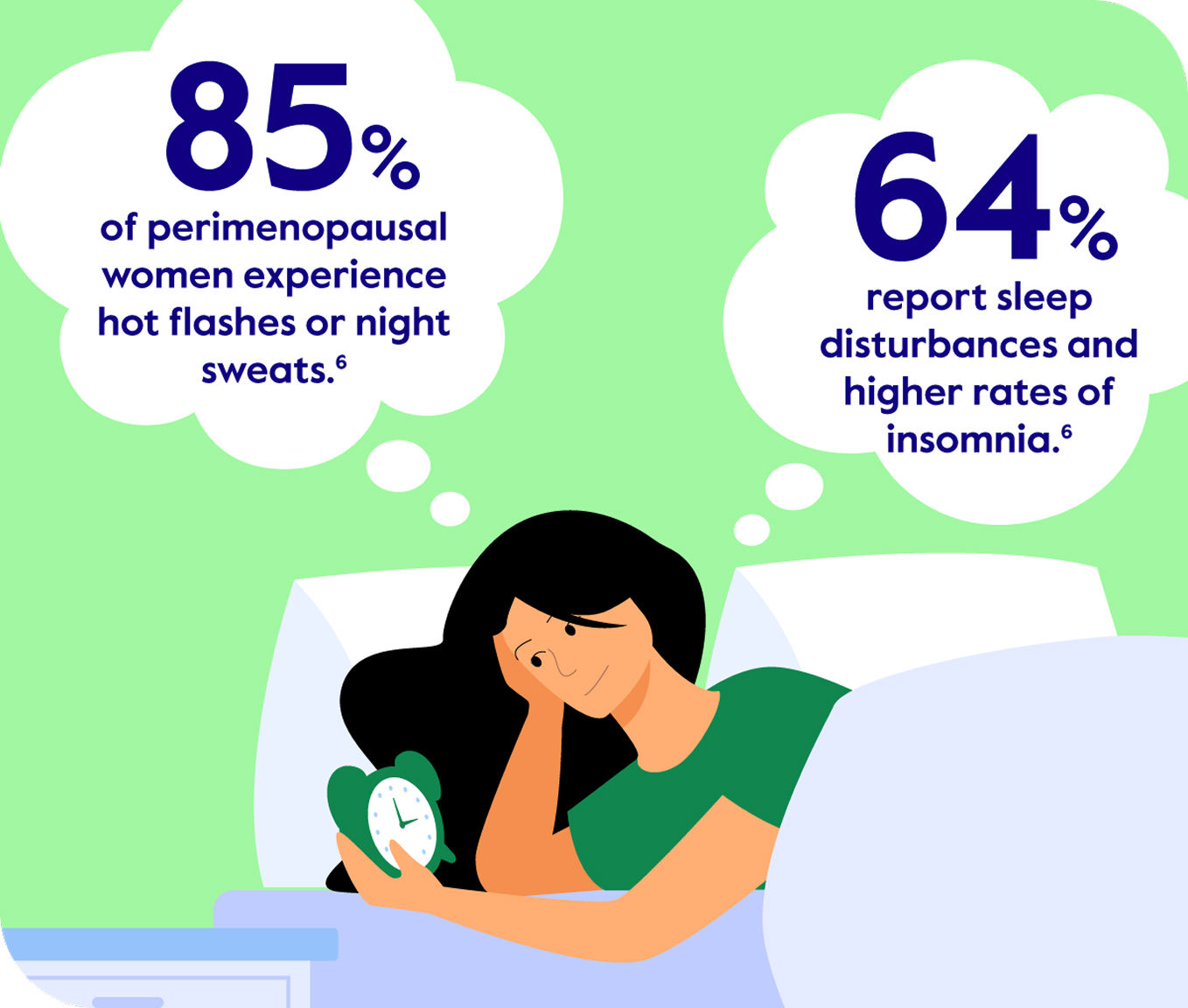
While menopause-related symptoms like night sweats and mood swings can lead to sleep problems, the opposite is also true. Poor sleep can increase hot flashes, night sweats, forgetfulness and other symptoms. Making a few healthy changes can help.
Sleep tip
Try to avoid common night sweat triggers, such as alcohol, spicy foods and caffeine. For additional help managing perimenopausal symptoms, talk to your doctor about treatments, such as hormone replacement therapy (HRT).
You’ve heard all the tried-and-true tips for getting better sleep. Eat right. Exercise. Don’t drink caffeine too late in the day. Here are a few ideas you may not have thought of.
- Practice “4-7-8 breathing.” If you find yourself waking in the middle of the night, this method can help slow your heart rate and give you something else to focus on besides not sleeping. Start by breathing in for 4 seconds, holding for 7 seconds and breathing out slowly for 8 seconds.
- Try “habit stacking.” Take an old habit you do every day, like brushing your teeth, and add a new habit on top of it, like taking a warm bath or meditating. Give it time. It can work.8
- Get morning light to sleep better at night. Getting a dose of natural light early in the day can help normalize your circadian rhythm when it’s time for bed. (Who knew?)
- Reserve your bed for sleep and sex only. While reading a book before lights out is ok, scrolling on your phone or computer is a no-no. Blue light from your devices can mess with your circadian rhythm.
When to seek professional help
While we all experience trouble sleeping every now and then, it’s important to talk to your doctor if your sleep issues last more than three months or occur alongside other unexplained health issues. Find Care.
Get better sleep with help from Visana.
Your medical plan includes access to Visana, a virtual women’s health clinic.9 Schedule a phone or video consultation for help with sleep issues, anxiety, night sweats and more. Booking appointments is quick and easy.
- Centers for Disease Control and Prevention (CDC). “Sleep Difficulties in Adults.” Last reviewed June 22, 2022. https://www.cdc.gov/nchs/products/databriefs/db436.htm
- Cleveland Clinic. “Why Women Need More Sleep than Men.” November 15, 2024. https://health.clevelandclinic.org/why-women-need-more-sleep
- Bryan L. “Insomnia and Women.” Sleep Foundation. Updated March 25, 2024. https://www.sleepfoundation.org/insomnia/insomnia-women
- Summer JV. “Sleep Apnea in Women.” SleepApnea.org. Updated November 5, 2024. https://www.sleepapnea.org/sleep-health/sleep-apnea-in-women
- Johns Hopkins Medicine. “Depression and Sleep: Understanding the Connection.” Last accessed April 11, 2025. https://www.hopkinsmedicine.org/health/wellness-and-prevention/depression-and-sleep-understanding-the-connection
- Bryan L. “How Can Menopause Affect Sleep.” Sleep Foundation. Updated January 18, 2024. https://www.sleepfoundation.org/women-sleep/menopause-and-sleep
- Harvard Health. “Blue light has a dark side.” July 24, 2024. https://www.health.harvard.edu/staying-healthy/blue-light-has-a-dark-side
- Cleveland Clinic. “Everything You Need to Know About Habit Stacking for Self-Improvement.” June 18, 2024. https://health.clevelandclinic.org/habit-stacking
- This service is offered as part of your Cigna Healthcare medical plan. Standard copays or coinsurance will apply.




